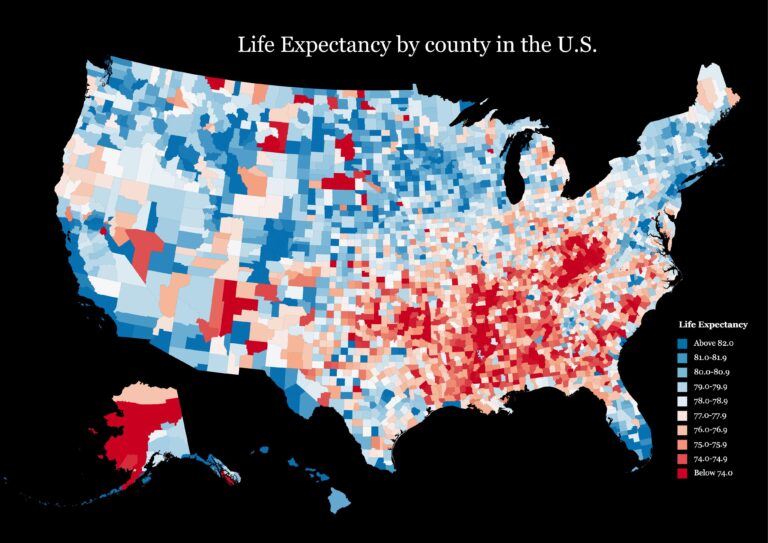
A new study published in The Lancet sheds light on the deep disparities in life expectancy across the United States, revealing how geography and education combine to shape health outcomes. Analyzing data from 2000 to 2019, the observational analysis uncovers significant gaps in longevity between counties and across levels of educational attainment, highlighting the enduring impact of social determinants on American life expectancy. The findings underscore the urgent need for targeted policies to address these inequalities and improve health equity nationwide.
Disparities in Life Expectancy Across US Counties Reveal Deep Educational Gaps
Recent findings highlight a striking correlation between educational attainment and life expectancy across counties in the United States from 2000 to 2019. Individuals with higher levels of education consistently enjoy longer life spans, with disparities reaching up to 15 years when comparing those with less than a high school diploma to college graduates. This gap signals entrenched socioeconomic and health inequalities that are geographically uneven. Counties with lower average educational attainment frequently grapple with limited healthcare access, higher prevalence of chronic diseases, and economic instability, factors that compound into reduced longevity.
The data pinpoint several critical patterns:
- High education counties often coincide with urban centers boasting robust healthcare infrastructures.
- Lower education counties are disproportionately rural, experiencing systemic barriers to quality education and preventive health services.
- Economic and social determinants such as poverty, employment, and health behaviors amplify these life expectancy discrepancies.
Addressing these disparities demands multidimensional strategies prioritizing educational equity and healthcare accessibility, tailored to the unique conditions of each county.
| County Category | Average Life Expectancy (Years) | Education Level (Adults 25+) |
|---|---|---|
| High Education Urban | 81.2 | Ōēź Bachelor’s Degree: 45% |
| Mid Education Suburban | 77.0 | High School Diploma: 65% |
| Low Education Rural | 69.8 | < High School Diploma: 35% |
How Educational Attainment Drives Health Outcomes Over Two Decades
Over the past two decades, the link between educational attainment and health outcomes has become increasingly pronounced, revealing deep-rooted disparities across U.S. counties. Individuals with higher levels of education consistently exhibit longer life expectancies, a trend that has widened rather than narrowed from 2000 to 2019. This divergence underscores how education functions not only as a marker of socioeconomic status but also as a critical determinant of health, influencing access to resources, health literacy, and preventative care practices.
Key factors driving this association include:
- Health behaviors: Those with more education tend to engage in healthier lifestyles, including lower smoking rates and better nutrition.
- Economic stability: Higher education often leads to better job opportunities and incomes, enabling access to quality healthcare.
- Healthcare access: Educated individuals are more likely to seek regular medical care and adhere to treatment regimens.
| Education Level | Average Life Expectancy (years) | % Change (2000ŌĆō2019) |
|---|---|---|
| Less than High School | 72.4 | +0.5% |
| High School Graduate | 76.9 | +2.2% |
| Some College | 79.8 | +3.5% |
| Bachelor’s Degree and Above | 83.6 | +4.1% |
Policy Implications for Addressing Regional Life Expectancy Inequalities
Addressing the stark disparities in life expectancy across counties and educational levels demands a multifaceted policy approach that targets both social determinants and healthcare access. Policymakers must prioritize investments in education and social services, recognizing the profound impact of educational attainment on longevity. Enhancing early childhood education, expanding access to quality higher education, and reinforcing adult learning programs are critical levers to close regional health gaps. Furthermore, expanding Medicaid and increasing funding for community health centers in underserved areas can improve preventative care and chronic disease management, mitigating mortality risks linked to socioeconomic disadvantage.
Effective strategies should also incorporate community-based interventions tailored to the unique challenges faced by lower-education populations in high-risk counties. Examples include:
- Localized health education campaigns that address modifiable risk factors
- Job training programs to improve economic stability and health outcomes
- Infrastructure improvements promoting safe neighborhoods and recreational spaces
- Policy frameworks fostering affordable housing and food security
| Policy Area | Target Benefit | Potential Impact |
|---|---|---|
| Education Access | Raise graduation rates | Increase life expectancy by 3ŌĆō5 years |
| Healthcare Expansion | Reduce untreated chronic diseases | Improve survival rates in vulnerable groups |
| Economic Support | Enhance employment opportunities | Lower mortality linked to poverty |
Investing in Education as a Key Strategy to Enhance National Longevity
The correlation between educational attainment and life expectancy highlights a crucial pathway for policy intervention. Research consistently demonstrates that individuals with higher education levels tend to enjoy longer, healthier lives. Investing in education extends beyond improving academic outcomes; it acts as a powerful determinant of public health, reducing disparities across regions and populations. Counties with greater proportions of college-educated residents show not only increased longevity but also lower rates of chronic diseases and better access to healthcare. This evidence supports the idea that education equips individuals with knowledge, resources, and social advantages that contribute to sustained well-being.
To capitalize on these findings, governments and stakeholders should prioritize policies that enhance educational opportunities, especially in underserved areas. Such strategies may include:
- Expanded funding for early childhood education and public schools to build foundational skills and reduce dropout rates.
- Scholarship and grant programs targeting low-income students to increase college enrollment and completion.
- Community-based educational initiatives that integrate health literacy and lifelong learning to promote healthier lifestyles.
These measures contribute to a virtuous cycle where improved education leads to healthier populations, lowered healthcare costs, and stronger economic prospects for the nation as a whole.
| County Education Level | Average Life Expectancy (Years) |
|---|---|
| High School or Less | 74.5 |
| Some College | 78.3 |
| BachelorŌĆÖs Degree or Higher | 82.7 |
In Conclusion
In summary, the groundbreaking analysis published in The Lancet highlights stark disparities in life expectancy across U.S. counties, closely tied to educational attainment levels from 2000 to 2019. The findings underscore how education remains a critical determinant of health outcomes, revealing persistent geographic and socioeconomic inequalities. As policymakers and public health officials grapple with these challenges, the study offers crucial data to guide targeted interventions aimed at narrowing the life expectancy gap and promoting equitable health opportunities nationwide.